Tackling tuberculosis: New models for an old disease
On World TB Day, Lucy Bell, from University College London, explores the research which has driven forward our understanding of TB today, and how cutting-edge research techniques are suggesting new strategies for TB treatment.

Each year on World TB Day, clinicians, researchers and policymakers take stock of the challenge still remaining in the fight against tuberculosis (TB). WHO figures show that 9.6 million people developed active TB in 2014, resulting in 1.5 million deaths from the bacterial infection. Among HIV-positive individuals, TB is the leading cause of death. Estimates suggest that up to a third of the world’s population are latently infected with TB – with no evident illness resulting from TB, but with a lifetime risk of reactivation and active infection. Significant challenges are faced in treating TB clinically: at least 6 months of antibiotics are required, with associated toxic side-effects. Increasingly high rates of antibiotic resistance also pose a rapidly evolving problem worldwide.
The date on which we recognize World TB day commemorates the March 24th, 1882, announcement by Robert Koch that he had isolated the causative infectious agent of TB: the tubercle bacillus. This seminal finding paved the way for 150 years of research into TB.
We now know that there is a complex relationship between the bacteria and the infected individual, in which the immune system plays a vital role. The site of TB infection (known as the granuloma), is a battleground on which the TB mycobacteria fight to replicate inside immune cells, macrophages, while these same cells co-ordinate with other parts of the immune system (including CD4+ T cells) in an attempt to kill and control the bugs. This stormy interplay leads to the inflammation and tissue destruction which causes TB disease.
Elegant work in the late 20th century began to hone our understanding of this host-pathogen interaction. Genetic studies in patients who were hyper-susceptible to TB-related infections identified deficiencies in the cytokines interferon-gamma and IL- 12, showing these factors to be essential in controlling mycobacterial infections. Studies in mouse strains bred to be deficient in these cytokines also demonstrated their critical role, and began elucidating the mechanistic basis of how they contributed to containing TB in vivo.
Nonetheless, huge questions remained unresolved in understanding TB pathogenesis. The fact that most people with active infection produced anti-TB interferon-gamma responses, but still failed to control the infection, suggested that it was necessary but not sufficient for protection – so what exactly did constitute an effective immune response? And what accounted for the disease heterogeneity where some people rapidly developed active TB after being infected, whereas some contained it as a latent infection?
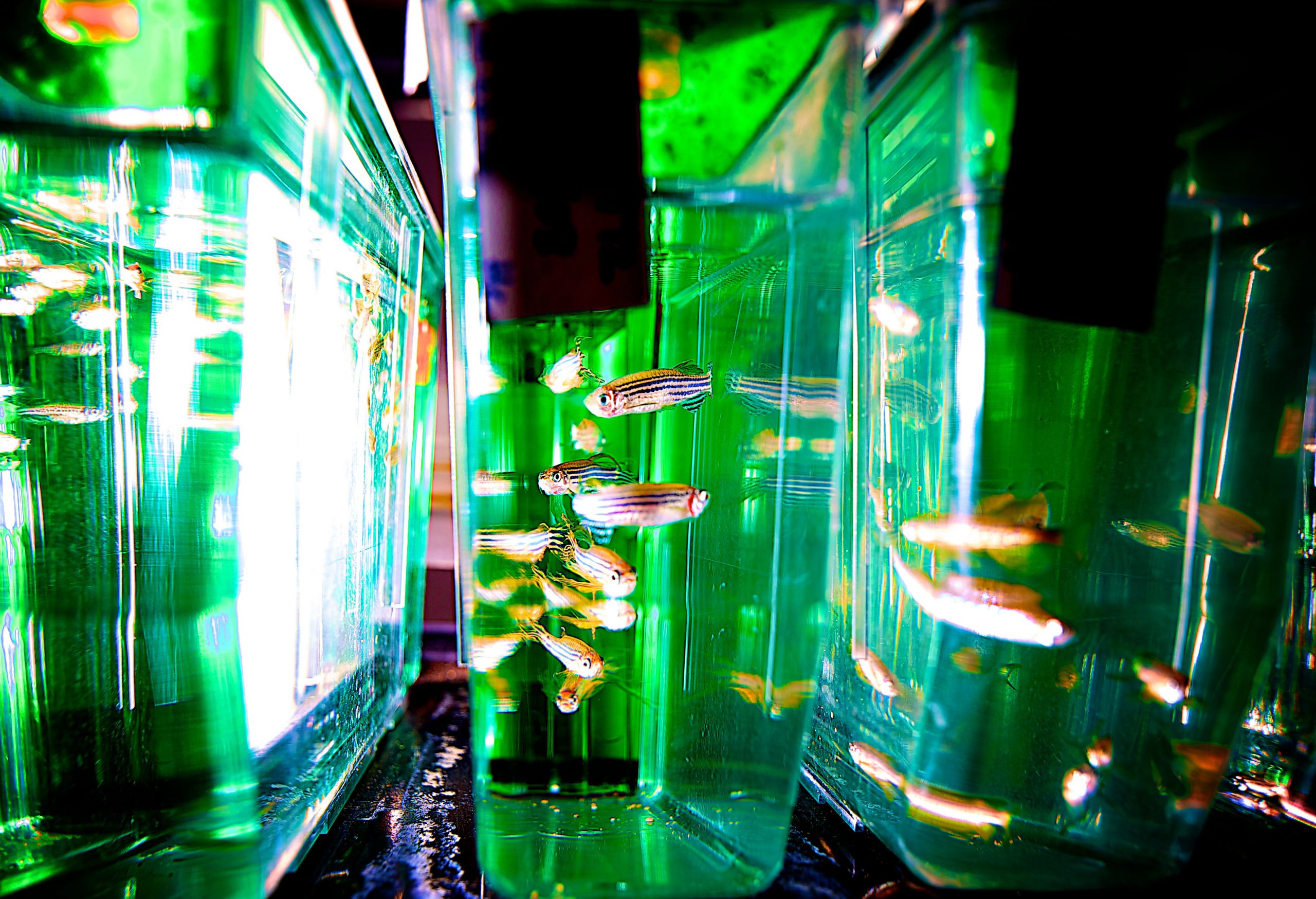
Excitingly, novel ways of studying TB have emerged, providing answers to these questions and accelerating progress in the field. By studying a natural host-pathogen interaction in the tiny zebrafish, which can be infected by a TB-like bug, Mycobacterium marinum, researchers defined a key characteristic of mycobacterial infection: either too much, or too little, inflammation causes disease, via tissue destruction or uncontrolled growth respectively, whereas a just-right amount of inflammation allows control; a so-called “Goldilocks effect”. They found that a human genetic locus, equivalent to that involved in the zebrafish, determined outcomes in a clinical trial of steroids in TB meningitis in humans. The idea of trying to therapeutically “balance” inflammation to treat TB emerged, and studies in mice have provided proof-of-concept for this strategy. The role of angiogenesis in mycobacterial infection has also been explored in zebrafish, identifying this process as another potential therapeutic target.
One key study in macaques used a combination of molecularly-barcoded bacteria and PET/CT scanning to characterise differences in TB control existing not only between hosts, but also within one single host – where different sites of infection showed a huge spectrum of disease activity. This model strikingly showed that local responses at the site of infection are critical in determining disease outcome, which could be a key consideration in fields such as vaccine design. PET/CT scanning has also been used in humans to investigate early treatment responses to novel anti-TB agents.
And although the most recent large TB vaccine trial didn’t find a protective vaccine effect, the development of advanced methods for looking at the effects of vaccines while still in early development is identifying promising new candidates. Methods include assessing the quality of vaccine-induced immune responses, and measuring their anti-microbial potency through a novel BCG challenge method – potentially repurposing the old sub-effective vaccine in a hunt for a new one.
Technologies allowing systems-level assessment of the immune response in humans, primarily via transcriptomics, have enhanced our ability to understand TB at the molecular level in vivo. Studies in this area have identified key characteristics defining active disease in contrast to latent infection and potential novel ways to diagnose TB, and in work I’ve been involved in, helped elucidate how HIV infection dramatically increases the risk of developing active TB.
Undoubtedly models will continue expanding our understanding of the disease, but it seems clear that there must be a strategy for identifying how research will translate to real outcomes for the millions of people affected by TB. In 2015, a call to action was made by a large cohort of TB researchers, to form an initiative aimed at expediting clinical studies of the various ‘host-directed therapies’ identified in basic research as candidates for optimising the anti-TB immune response. Alongside progress in the vaccine field, these avenues have the potential to revolutionise the treatment of TB in the coming decades; lighting the way to aim for the UN Sustainable Development Goal of ending the TB epidemic by 2030.
 Lucy Bell (@LucyCKBell) received her PhD from University College London in 2014, where she carried out her research in the Noursadeghi lab, studying the impact of HIV co-infection on immune responses to TB using in vitro macrophage models and in vivo transcriptomic studies in TB patients. She is currently completing her medical degree at UCL and is hoping to embark on a career as a clinician scientist working on infectious diseases. She has no conflicts of interest.
Lucy Bell (@LucyCKBell) received her PhD from University College London in 2014, where she carried out her research in the Noursadeghi lab, studying the impact of HIV co-infection on immune responses to TB using in vitro macrophage models and in vivo transcriptomic studies in TB patients. She is currently completing her medical degree at UCL and is hoping to embark on a career as a clinician scientist working on infectious diseases. She has no conflicts of interest.