The Global Response to the Ebola Fever Epidemic: What Took So Long?
Mark J. Siedner of Harvard Medical School and John D. Kraemer of the O’Neill Institute for National and Global Health Law, Georgetown University, discuss the impact of the delayed global response to the Ebola epidemic.
On August 8, twenty weeks after the first suspected cases in what has become the worst hemorrhagic fever outbreak in history, the World Health Organization’s (WHO) Director-General declared the epidemic a public health emergency of international concern (PHEIC). The announcement, which signals that an epidemic constitutes a sufficient public health risk to member WHO States through the spread of disease, will ideally motivate financial and logistic support to the countries most affected. But after nearly 1,000 deaths, and for a disease where a relatively simple and coordinated public health response has extinguished prior epidemics, many are left wondering, “what took so long?”
An integral part of the WHO mission, mandated by the International Health Regulations (IHR), is to protect member states from international public health threats. The IHR were revised in 2005 after the SARS outbreak to improve responses to epidemics in an increasingly globalized world. Among the IHR’s central components is commitment from high-income countries to build capacity to prevent public health emergencies, and to provide assistance during active ones. The IHR task WHO with promptly identifying emergencies by declaring PHEICs to sound the proverbial alarm.
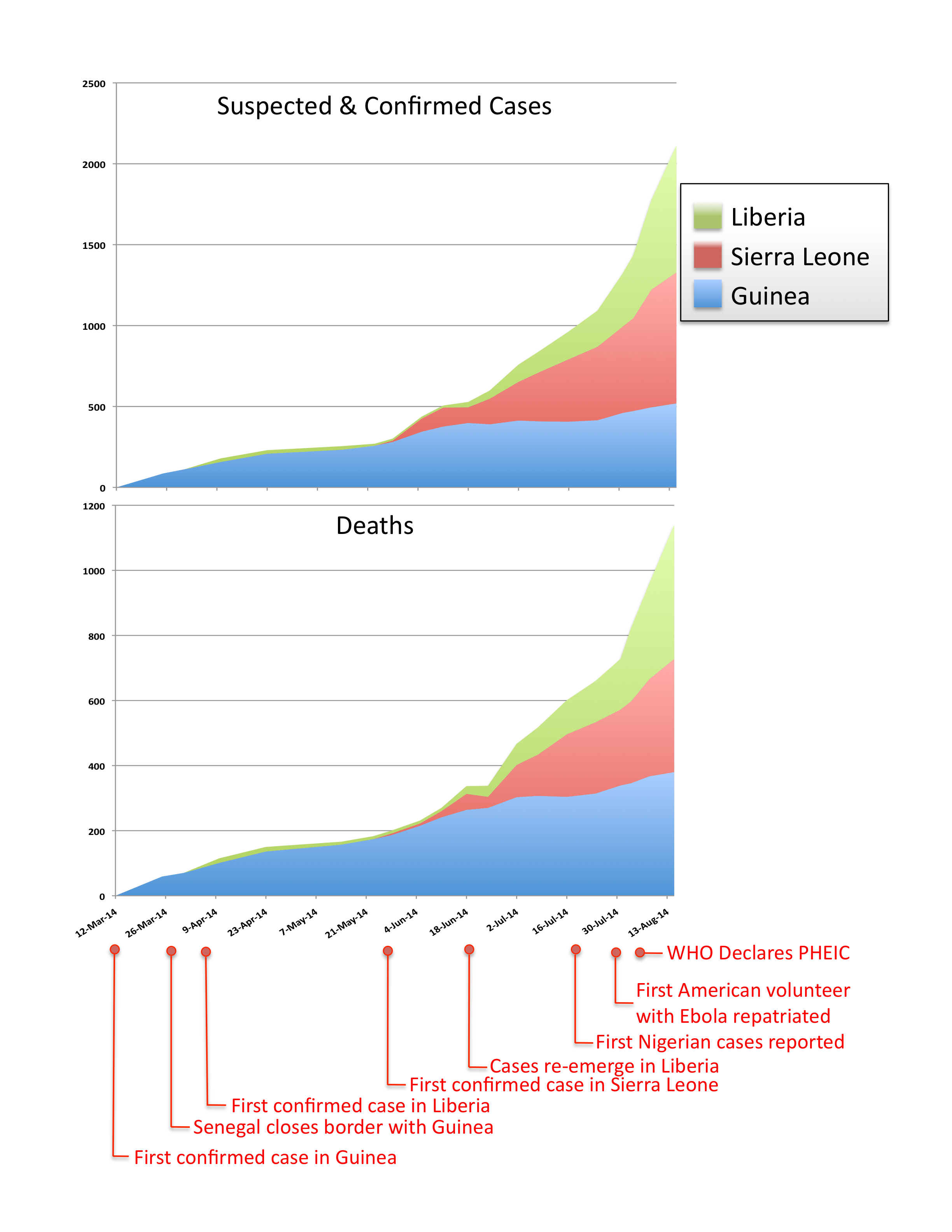
By most accounts, the criteria to declare a PHEIC were met months ago (Figure 1). The outbreak quickly made public health impact with its rapid pace and case fatality rates above 50% and by disproportionately affecting healthcare workers. It became an international epidemic five days after the first cases were reported when it spread from Guinea to Liberia. The epidemic is also unusual because it represents the first hemorrhagic fever epidemic in urban areas, where poverty and population density exacerbate disease spread. Only nine days after Guinea notified the WHO of the outbreak, Senegal closed its land borders with Guinea. By the end of May – 10 weeks before the PHEIC declaration – the epidemic raged on in Guinea, gained speed in Sierra Leone, and reemerged in Liberia.
In hindsight, the greatest lapse in judgment by the international public health community was over-reliance on a heroic, albeit underfunded effort by local governments in partnership with multinational partners. Sierra Leone and Liberia are post-conflict states with health systems decimated by war. Since the start of the outbreak, the Liberian legislature has authorized $20 million USD of domestic resources to respond to the outbreak—3.5% of its national budget. Despite these investments, the country has struggled with basic containment measures, including supplying healthcare workers with personal protection equipment (PPE), ensuring safe burial practices, tracing contacts, and establishing secure quarantine. As of July, in Liberia there was only a single case detection team, insufficient funds to compensate healthcare workers, lack of fuel for contract tracing or to operate the reference laboratory, and body bags were in short supply. As standard measures floundered, governments turned to extraordinary social interventions, including closures of schools and government buildings, and a military-enforced cordon sanitaire at border areas.
It was not until the end of July, as cases reached more affluent shores, that the Ebola outbreak gained visible international profile. Two American aid workers were infected and eventually flown home for care. Unfounded criticism of the decision to repatriate them was in large part responsible for disseminating news of the epidemic in the West. Almost simultaneously, an airline passenger died of Ebola just after arriving in Lagos, sparking a rash of cases in Nigeria. While risk of significant transmission remains highly unlikely in countries with effective public health infrastructure, these events spurred concerns about a worldwide threat.
Shortly thereafter, a concerted international response began to take shape. In the past two weeks the WHO has pledged to raise $100 million, the World Bank has committed $200 million in emergency aid, and CDC committed to a substantially increased presence. Médecins sans Frontières, which has been among the most active aid groups from early in the epidemic, have mobilized almost 700 personnel, including every hemorrhagic fever expert within the organization. On August 6th, the WHO finally convened an emergency committee, which unanimously recommended that PHEIC declaration.
The delay in action has been devastating. The most obvious cost has been the lives of those unnecessarily taken by Ebola. Since the beginning of the second wave of cases in May, over 1600 Ebola cases and 850 deaths have occurred. Sadly, these represent a fraction of the deaths that will result from this outbreak. Scores of healthcare workers without adequate PPE or oversight have abandoned their posts. Meanwhile, as the epidemic has spread, it has brought stigma and distrust of healthcare workers, closing of public hospitals in the height of the malaria season, and leveling of what little public health infrastructure existed in the region. The long-term consequences of the epidemic are even more dire. At least 150 healthcare workers have been infected and more than 75 have died. In Liberia, which had an estimated 50 physicians and 1,000 nurses as of 2008, 85 healthcare workers have been infected and 35 have died while selflessly caring for the ill. The catastrophe of their collective loss will reverberate for decades.
The IHR were designed to create a system of collective health security in which the global community responds vigorously to emergencies across international borders. If we value the security promised by this system, we owe a reciprocal duty to follow through on commitments made to low-income partners. Though their capacity was limited, Liberia, Guinea, and Sierra Leone met their international obligations. In the future, we as a global public health community must extend collective security to all WHO member states, not only when we perceive a threat to high-income interests.
About the authors: Mark J. Siedner, MD, MPH is an Instructor of Medicine at Harvard Medical School and a Research Scientist at the Center for Global Health at Massachusetts General Hospital. John D. Kraemer, JD, MPH is a Scholar at the O’Neill Institute for National and Global Health Law and Assistant Professor in the Department of Health Systems Administration at Georgetown University.

[…] outbreak has had a slow and unimpressive response from governments in the affected countries and from the WHO. The heavily affected countries have incredible health care worker shortages and, as more health […]
[…] alle Ong (quelle vere), “The Global Response to the Ebola Fever Epidemic: What took so long?” gratis su PLoS Medicine, che parla anch’essa del crollo della sanità pubblica in […]
[…] ligt onder vuur. Ze hebben de uitbraak te laat serieus genomen, luidt de kritiek onder andere in dit artikel. Ook Koppens is teleurgesteld in de aanpak van de World Health Organization (WHO). ‘Wat er miste […]
[…] urban occurrence of hemorrhagic fevers in urban slums, in crowded areas where it dramatically spread, overwhelming health care workers whom it affected in great numbers, and the fear of its […]